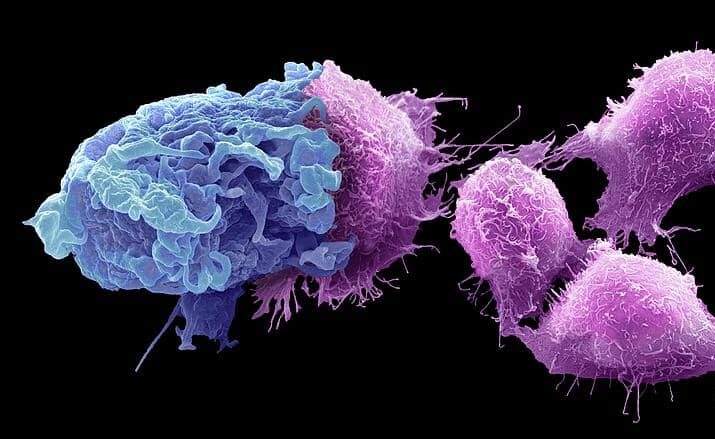
At Evolve, we love macrophages. Literally the “big eaters” of the immune system, macrophages are critical orchestrators of the immune response. Given the central role of macrophages in both cancer immunity and autoimmune disease, they would seem an ideal candidate for immune cell therapy. However, the therapeutic macrophage field is still very much in its infancy compared to the more established field of CAR-T therapy. There are unique challenges associated with manufacturing and engineering macrophages that need to be overcome if the therapeutic potential of these incredible cells is to be realised. However, this also means that there is considerable opportunity for pioneering innovators to capture valuable IP in the space.
Advantages of CAR-M Therapy
CAR-Macrophage (CAR-M) therapy has potentially significant advantages over CAR-T therapy. Unlike T cells, macrophages are naturally adept at trafficking into and surviving within solid tumour masses. Additionally, the role of macrophages as the orchestrators of the immune response means that CAR-M therapy could deliver a multi-pronged mechanism of action, involving direct tumour killing via phagocytosis, tumour Microenvironment (TME) remodelling, and activation of adaptive immunity, including T cells. It is also hoped that the distinct mechanisms of action of macrophages will contribute to a favourable safety profile. Indeed, early clinical trials have reported no dose-limiting toxicities or the severe cytokine release syndrome (CRS) and neurotoxicity (ICANS) that frequently limit CAR-T treatment. The enhanced safety of macrophages may make them an attractive option for both oncology and autoimmune disease.
Beyond oncology, the unique capabilities of macrophages also make them attractive candidates for a range of other diseases. Macrophages are key regulators of tissue repair and fibrosis. Engineered macrophages are therefore being developed to deliver anti-fibrotic agents directly to scarred tissue in organs like the liver and lungs. CAR-based cell therapies are being explored to selectively eliminate the pathogenic B cells that drive many autoimmune disorders, with macrophages offering a potentially safer cellular vehicle. Preclinical work has also shown that CAR-Ms can be designed to target viral antigens, such as the SARS-CoV-2 spike protein, and mediate viral clearance without inducing the excessive inflammation associated with severe disease.
CAR-M design and function
Just like T cells, the macrophages for use in CAR-M therapy may be derived from a patient’s circulating monocytes or, for an allogeneic approach, may be differentiated from stem cells. The CAR constructs used in CAR-M therapy are also structurally analogous to those used in T cells, comprising an extracellular antigen-binding domain (most commonly a single-chain variable fragment, or scFv), a hinge region, a transmembrane domain, and one or more intracellular signalling domains. However, the intracellular domains of the CARs used in CAR-M are adapted to trigger biological functions inherent to macrophages. Instead of the lytic machinery activated in T cells, CAR-M signalling domains like FcRγ, CD3ζ, Megf10, or Toll-like receptor (TIR) domains are designed to initiate robust, antigen-dependent phagocytosis, primarily through signalling cascades involving pathways such as PI3K/AKT.
Key challenges in CAR-M development
There are clearly obvious clinical advantages of macrophages compared to T cells. However, the clinical success of CAR-macrophages will be dependent on the ability of innovators to overcome some key engineering and manufacturing challenges unique to these complex and heterogeneous cells. The first challenge for a CAR-macrophage cell therapy product is persistence. The functional plasticity that makes macrophages so adaptable also means CAR-Ms can have a habit of switching to an undesirable phenotype in response to environmental stimuli once administered to a patient. In cancer, the immunosuppressive tumour microenvironment (TME) can reprogram anti-tumour (M1) cells into a pro-tumour (M2) state. A successful CAR-M therapy must therefore use cells that are engineered for phenotypic stability.
Whilst manufacturing is a challenge for all cell therapies, making macrophages is particularly difficult. Compared to T cells, macrophages are not easy to culture and expand ex vivo. Importantly, unlike T cells which can easily be cultured in suspension, macrophages are sticky. This means that once a differentiated macrophage has stuck itself down to the culture dish, it can be very difficult to remove them without inducing some degree of cytotoxicity. Aligned with their function as the immune system’s sentinel cells, macrophages are also very sensitive and temperamental cells. Macrophages are consequently very difficult to engineer, transport and store. To make matters worse, macrophages are also particularly sensitive to innate immune stimuli, including components of the viral vectors often used to introduce the Chimeric Antigen Receptor expression cassettes. Engineering macrophages therefore requires highly cell-specific protocols and macrophage expertise.
Emerging innovations in CAR-M therapy
The challenges and opportunities represented by CAR-M therapy mean that there are considerable opportunities for developing and securing valuable IP. The differences between macrophages and T cells mean that many of the scientific and clinical strategies developed for CAR-T are not applicable to macrophages. This means that there is a need for considerable innovation in the field, with the potential to yield strong IP.
Notably, one of the leaders in the field, Carisma Therapeutics, has recently pivoted their strategy to streamline manufacturing and improve the persistence and tumour-trafficking capabilities of their therapy. Carisma’s first clinical candidate (an anti-HER2 CAR-Macrophage, CT-0508) was successfully validated for safety in Phase 1 but only demonstrated limited clinical efficacy. Carisma has therefore shifted their approach away from differentiated macrophages towards the use of monocyte precursors, with a new anti-HER2 CAR-M lead asset, CT-0525.
As with CAR-T cell therapy, there is also increased interest in in vivo engineering of macrophages, using technologies like mRNA-LNP delivery to create CAR-M cells directly within the patient. This strategy eliminates the need for complex ex vivo cell processing to potentially convert the treatment from a personalized, high-cost model into a scalable, “off-the-shelf” product. Notably, Carisma is advancing an in vivo engineering platform in a major collaboration with Moderna, using mRNA/LNP technology to target oncology (like GPC3) and autoimmune diseases. CREATE Medicines (recently rebranded from Myeloid Therapeutics) is also developing an in vivo technology based on mRNA-lipid nanoparticles (LNP). The company’s lead assets, MT-302 (targeting TROP2) and MT-303 (targeting GPC3), are currently in Phase 1 clinical trials for solid tumours, including glioblastoma and hepatocellular carcinoma.
To exploit the full potential functionality of macrophages, advanced cell engineering approaches are also being developed to produce “armoured” macrophages with improved functionality and persistence. Inceptor Bio, for example, is a US-based company developing a preclinical CAR-M platform approach focused on augmenting macrophages’ natural functions, engineering them to enhance tumour infiltration, boost phagocytosis, and bypass the CD47/SIRPα “don’t eat me” checkpoint
CAR-M Intellectual Property (IP) landscape
Given the significant challenges associated with manufacturing macrophages, it is unsurprising that significant IP has been filed directed to manufacturing processes, see for example Inceptor Bio’s pending international application directed to a method of manufacturing a myeloid-derived cell from stem cells (WO 2025046513 A1), and Carisma’s granted US patent for modifying ex vivo a CAR-macrophage comprising treating the macrophage with a CD40 agonist (US 11739297 B2). Interestingly, Carisma Therapeutics is a University of Pennsylvania spin-out, from which it licenses some foundational CAR-M IP. The granted US patent (US11498954 B2), for example, claims simply a modified macrophage or monocyte comprising a CAR exhibiting reduced SIRPα activity.
The unique properties and challenges of macrophage mean that there are also considerable opportunities in this field for protecting the product. Product IP is generally preferred, as it is easier to enforce and harder to design around (Evolve Insights). Product IP may be directed to, for example, the CAR itself, given that it must generally be optimised for use in macrophages versus T cells. See, for example, CREATE Medicines’ patent application directed to an anti-TROP2-expressing “chimeric fusion protein”, wherein the transmembrane domain of the protein dimerizes with endogenous FcR-gamma receptors expressed in myeloid cells, monocytes or macrophages.
The macrophages themselves may also be protected. Similarly, Inceptor Bio’s pending application WO 2024236547 A1 is directed to a CAR comprising a cytoplasmic domain of a herpes virus entry mediator (HVEM) protein. Patents may also be directed to macrophages themselves. Resolution’s pending application WO2024068728 A1, for example, relates to an engineered macrophage for use in treating fibrosis expressing the anti-inflammatory molecule MMP9.
Importantly, however, an IP strategy seeking to protect a CAR-M product must take account of the intrinsic heterogeneity of these cells. It is critical that the definition of the product in the claims is aligned with the detailed description of the patent and also with how the product is defined in regulatory documents and licensing contracts. Particular care must be taken when the product delivered to patients takes the form of a monocyte precursor (Evolve Insights).
As with in vivo CAR-T cell therapies, the shift to in vivo CAR-macrophage approaches also presents considerable opportunity for capturing valuable IP (Evolve Insights), including IP directed to the delivery vehicles and cell targeting approaches. However, innovators will also need to navigate the potential FTO risks. Notably, we have already seen an in vivo cell therapy company, Capstan (Abbvie), added to the ongoing LNP litigation.
As CAR-M products advance through the clinic, the pioneering nature of these therapies means that there are likely to be many opportunities for clinical IP, directed to doses, formulations, patient subpopulations, delivery methods, new therapeutic uses and combination therapies.
Outlook
CAR-Macrophage therapy therefore represents a bold new frontier in cell therapy, moving beyond the T-cell-centric model to harness the unique power of the innate immune system. These impressive cells promise enhanced safety and a multi-faceted attack on disease, particularly in solid tumours where other cell therapies have faltered. However, translating this promise into reality is a complex undertaking, demanding innovative solutions to the distinct challenges of macrophage engineering, manufacturing, and persistence. The field is already developing at pace, with strategies like in vivo mRNA-LNP delivery and the engineering of “armoured” cells bypassing traditional hurdles. This wave of specialist innovation means that there is also considerable opportunity to carve out a valuable and defensible intellectual property space, distinct from the increasingly crowded CAR-T field. However, IP strategy for advanced therapies such as CAR-M requires a deep understanding of both the product and the competitive landscape.
Are you a macrophage cell therapy innovator looking for strategic advice from someone with in-depth knowledge of both the science and IP landscape? We have the unique scientific and IP expertise that you need. We can particularly advise on due diligence, licensing, and freedom to operate, as well as providing drafting and prosecution support. Get in touch today!
Author: Rose Hughes

Rose is driven by a passion for science and combining scientific knowledge with practical IP solutions. Rose brings over a decade of pharmaceutical and biotech patent expertise to evolve, including both law firm experience and six years working in-house at AstraZeneca. Rose’s passion for science stems back to her PhD in immunology and infectious disease at UCL, working on the innate immune responses of macrophages to viral infection. Macrophages remain her favourite cell!.
At AstraZeneca, Rose led IP strategy for products at every-stage of the pipeline, including on-market assets. She was responsible for developing and executing the IP strategy for the biopharma cell therapy department and the neuroscience division. Rose has also completed due diligence and negotiated IP terms for high-profile transactions in the biopharma and oncology space, including cell therapy platform deals. Rose provides invaluable industry expertise to address the unique challenges of IP strategy in the life sciences sector.