Originally posted on IPKat.
IP strategy for cell therapies presents unique challenges compared to traditional pharmaceuticals and biologics. Previous posts have highlighted the limitations of process patents in cell therapy and the need to think strategically about how best to protect the product from fast-follower competition. This post focusses on an even more fundamental challenge, that of the inherent complexity of defining a cell and what this means for devising an effective IP strategy.
Why cells defy simple classification
Cell-based therapies face a definitional problem that is far more complex than for other types of drug such as small molecule pharmaceuticals and monoclonal antibodies. Small molecules can be precisely defined by their chemical structure, whilst antibodies can be characterized by their amino acid sequence. In contrast, cells exist in a state of remarkable complexity and inherent variability.
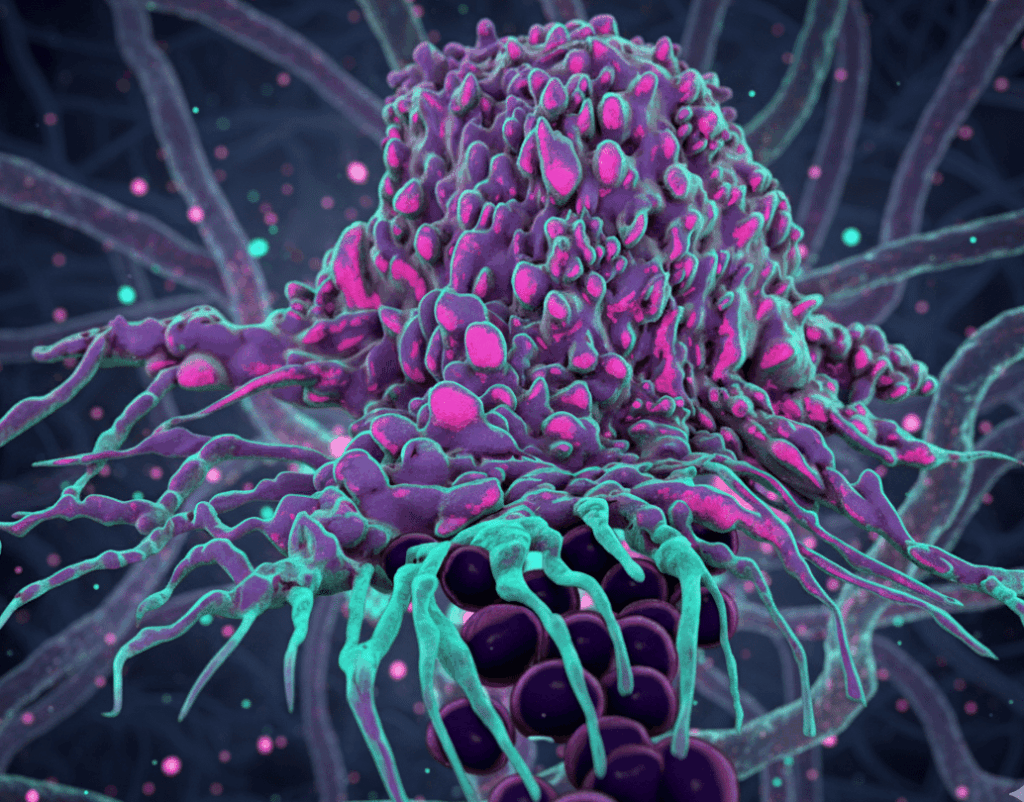
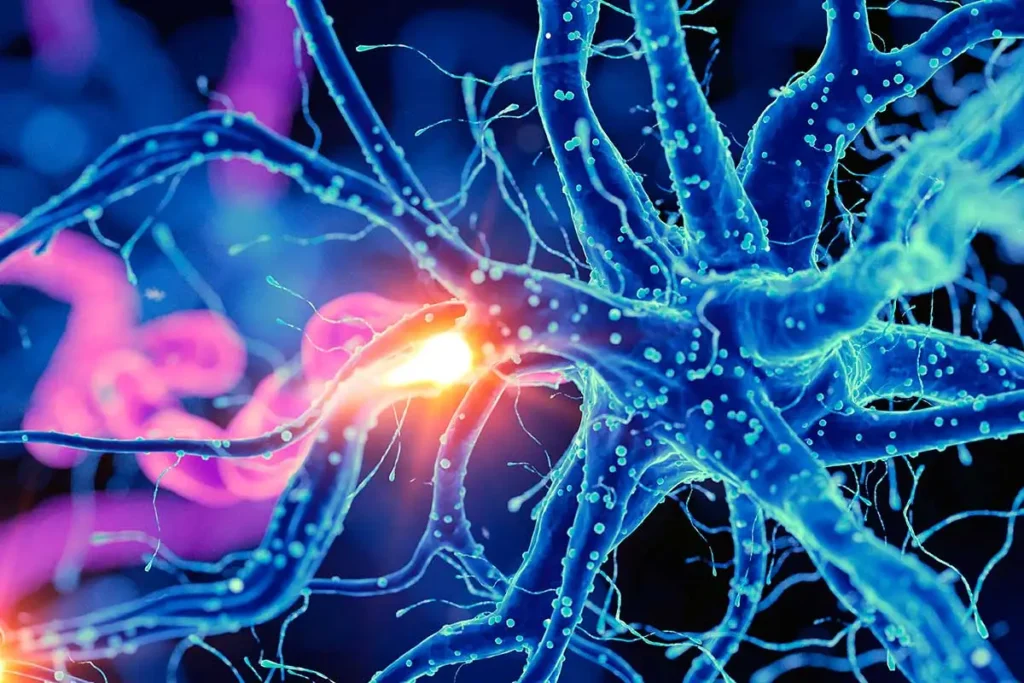
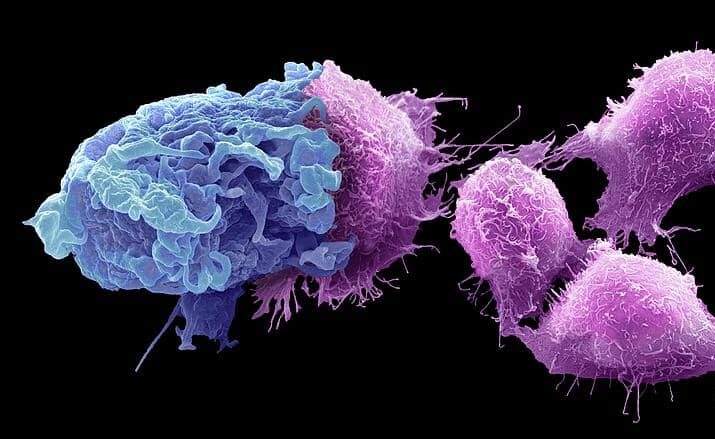
Many cell therapies are based on harnessing the body’s own immune cells to fight disease. However, cells of the immune system present a particular challenge with regards to finding a clear definition. The complexity of the immune system cannot be overstated. It comprises hundreds of distinct cell types across innate and adaptive immunity, each with specialized functions, characteristic marker profiles, and complex developmental lineages. This system has evolved over millions of years to provide flexible, overlapping mechanisms of defence against a vast array of potential threats. Scientists are continuously discovering new cell types and subtypes, each with increasingly nuanced functions. The explosion of single-cell RNA sequencing technologies has accelerated this trend, revealing unprecedented heterogeneity within what were previously considered uniform cell populations.
Macrophages! A lesson in complexity
To illustrate the problem with defining a cell type, we need look no further than my favourite cell, the macrophage. The basic definition of a macrophage is a specialist cell involved in the detection, phagocytosis and destruction of bacteria and other harmful organisms (think a cellular Pac-Man). Within the field of immunology, macrophages are identified by their appearance, their function and by their expression of certain cell surface proteins. However, macrophages are not a homogenous cell population, but a diverse family of immune cells that exist throughout the body, including specialized macrophages in the liver, brain, skin and other organs. Even beyond the tissue specific differences, macrophages exist along a functional spectrum with key activation states, including pro-inflammatory macrophages that produce inflammatory cytokines and fight pathogens, and anti-inflammatory macrophages (with various subtypes devoted to wound healing and tissue remodelling). Rather than fixed categories, these macrophage types represent a continuum with significant plasticity, allowing macrophages to adapt their function based on environmental cues and switch phenotypes during disease progression or resolution.
Unlike a chemical entity that can be defined by its structure in a patent claim with precision, immune cells can thus only be defined by a combination of functional characteristics and surface marker expression patterns that generally exist on a continuum rather than as discrete categories. However, even the measurement of cell surface markers is often far from clear-cut. The standard techniques in the field for identifying populations of cell types, such as fluorescence-activated cell sorting (FACS) plots, measure varying levels of expression on a continuous scale. The boundaries of what defines the cell population can often be fuzzy.
Macrophages are also far from the most complex family of immune cells. Most immune cell types, including B cells, T cells and NK cells, have a similar or greater degree of complexity. The heterogeneity of cellular gene expression within certain cell types creates a significant challenge when attempting to provide precise legal definitions of cell types in patent claims or contracts. Where exactly does one cell type end and another begin? The boundaries are often blurred and context-dependent.
Lab versus reality
To make the problem of defining a cell even more challenging, cells grown in the lab can also exhibit markedly different phenotypes depending on their differentiation conditions. It can be unclear which differentiation conditions most accurately reflect the “real” cell type in the body. Tissue cell lines, widely used in early stage research, present another layer of complexity. These immortalized cell populations derived from primary tissues provide convenient laboratory models but may not accurately reflect the functionality of their in vivo counterparts. Macrophage-like cell lines, for example, often lack key functional characteristics of primary macrophages such as robust type I interferon responses essential for antiviral defence, making these cell lines borderline useless for evaluating host-pathogen interactions.
The discrepancy between lab-cultured cells and the cells in the body can have profound implications for drug discovery and development. Compounds that show promise in cell line studies may fail when tested in primary cells or in vivo due to these functional differences. This creates significant challenges when attempting to define cellular targets for disease or when specifying the cells that a therapy is designed to modulate.
Mouse versus human
Adding further complexity to the cell definition problem is the fact that the mouse immune system, where most initial drug testing occurs, differs substantially from the human immune system. Mice and humans have evolved important immunological differences, in some of the most key immune pathways and responses. These differences mean that cellular definitions that work well in mouse studies may require significant translation when applied to human therapies. A therapy targeting a specific immune cell subset in mice might find that the equivalent human population has different markers, functions, or regulatory mechanisms.
Implications for IP and licensing: Complex problems require creative solutions
This biological complexity creates significant challenges for IP strategy and licensing agreements in the cell therapy space. How can one precisely define a cellular product when the very definition of the cells involved is subject to ongoing scientific refinement? For patent drafting, the challenge lies in crafting claims that are both specific enough to be valid and broad enough to provide meaningful protection. Overly specific definitions of cell types risk becoming outdated or easily circumvented as the product moves through the clinical pipeline. By contrast, overly broad definitions may lack the specificity required for patent validity or lead to the challenge that the claims are not sufficiently supported by the data. Additionally, as we know from the case at issue in G 1/24, inaccurate definitions in a patent specification can lead problematic interpretation of claim scope for the patentee.
Similar challenges arise in collaboration, licensing and acquisition agreements. How do you define the technology being acquired or in-licensed when the underlying cellular definitions are fluid? Defining a cell type too narrowly in the license or collaboration agreement may lead to the eventual product falling outside of the definition. Defining a cell type too broadly may inadvertently capture technology that one party did not intend to fall under the scope of the deal.
IP strategy for cell therapy technologies must therefore constantly adapt to ever evolving complexity of the science. At every stage of the product lifecycle, it is important to focus on how the product may be defined by both function and markers. Both of these characteristics of a cell therapy product may be used to obtain meaningful protection in a patent or protect a party’s interests in a contract. The characteristics that will provide the most meaningful protection are those that can be linked with the clinical product, as defined by the regulatory authorities. Prior to a regulatory filing, it is essential for the IP strategy to prepare for the fact that the definition of a cellular product may evolve over time as the science develops.
Final Thoughts
Cell therapies exist in a realm where definitions are provisional, boundaries are blurred, and our understanding of the underlying science constantly continues to evolve. Successfully navigating this complexity requires a combination of scientific sophistication, legal creativity, and strategic foresight. By acknowledging the inherent limitations of cellular definitions while developing flexible approaches to product protection, companies can build IP strategies that accommodate the wonderful complexity of the immune system. In order to ensure robust and meaningful protection, effective IP strategies for cell therapies need to acknowledge and harness the remarkable complexity of cellular products they aim to protect.
Author: Rose Hughes